Pennie’s got you covered
Pennie is here for you
Pennie is here for those who lost or are losing Medicaid, also known as Medical Assistance (MA) coverage. Check out our video below that explains how Pennie can help!

Pennie gets you covered
If you are ineligible for Medicaid, you may be referred to Pennie, Pennsylvania’s official health insurance marketplace. At Pennie you can shop for plans available in your area. Pennie is the only place to get financial savings to help pay for coverage.
You Did Not Respond To Your Packet
If you do not respond to the renewal packet and therefore lose your Medicaid coverage, Pennie will contact you with information on coverage options.
Visit the enroll webpage for simple instructions on how to enroll in coverage through Pennie. Choose the Qualifying Life Event, “Loss of Medicaid or CHIP” to shop for plans.
IMPORTANT NOTE: Pick a health plan within 90 days from the date you lost Medicaid coverage
You Responded To Your Packet
If you respond to your renewal packet and are found ineligible for Medicaid, your account will be automatically and securely transferred to Pennie. A pre-filled application will be created on your behalf, and you will receive a notice with a unique access code for your new Pennie account and an estimate of financial savings to lower the cost of coverage. You will have a limited time to shop for coverage through a Special Enrollment Period. This shopping window will be available already for some customers, or you can select “Loss of Medicaid/Medicaid or CHIP” when asked.
IMPORTANT NOTE: Pick a health plan within 90 days from the date you lost Medicaid coverage.
Frequently asked questions
What is Pennie?
Pennie is the Commonwealth of Pennsylvania’s official health insurance marketplace where individuals and families can apply for, shop, and enroll in health coverage that best fits their needs. Pennie is also the only link to financial savings to help reduce the cost of monthly premium payments and/or out-of-pocket costs.
Pennie works closely with the Pennsylvania Department of Human Services (DHS), the Office of Income Maintenance (OIM), and the Children’s Health Insurance Program (CHIP) to develop a “no wrong-door policy. This policy seamlessly transfers applications for those who are eligible for Pennsylvania’s Medicaid and CHIP programs. In addition, applicants who are denied Medicaid (and likely eligible for marketplace coverage) are transferred by DHS to Pennie to apply and enroll.
I currently have Medicaid coverage and haven’t received a renewal packet; is there anything I should be doing to make sure I am receiving all of the appropriate paperwork?
The best thing you can do now is to make sure your contact information and address are up to date with the Pennsylvania Department of Human Services (DHS). You can update your information through COMPASS and sign up for text or email alerts to get information faster when it is your time to renew. If you cannot access COMPASS, you can update your contact information by calling the Customer Service Center at 1-877-395-8930 or 215-560-7226 in Philadelphia.
Watch for mail, emails, and texts from DHS. Messages from DHS are sent to inform you of important actions needed for your benefits or to let you know about valuable programs that could be of assistance to you and your loved ones.
You should be on the lookout for your Medicaid renewal packet in the mail. Once you receive your packet, you will need to complete and return it to your local County Assistance Office by the due date listed in one of the following ways:
- In-person drop-off
- Fax
- In-person drop-off (in the office or via drop box, if the office has one)
You can also complete your renewal online from our COMPASS site at dhs.pa.gov/COMPASS. You can even submit any necessary verification documents on COMPASS or through the myCOMPASS PA mobile app.
I currently have Medicaid coverage, what happens if I do not submit my renewal packet and/or verification documents by the due date?
If you do not return your renewal or do not provide the requested verification by the due date, your Medicaid coverage will close. You will receive a notice which includes your appeal and fair hearing rights and instructions for filing an appeal. You can also still give us your renewal and/or verification documents up to 90 days after the date your MA closes on your notice. If you are still eligible for MA, your MA will reopen with no gap in coverage.
Visit the Department of Human Services Public Health Emergency webpage for more information: Public Health Emergency and Medical Assistance (pa.gov).
If I do not respond to my renewal packet and my Medicaid coverage ends, how do I enroll in health coverage through Pennie?
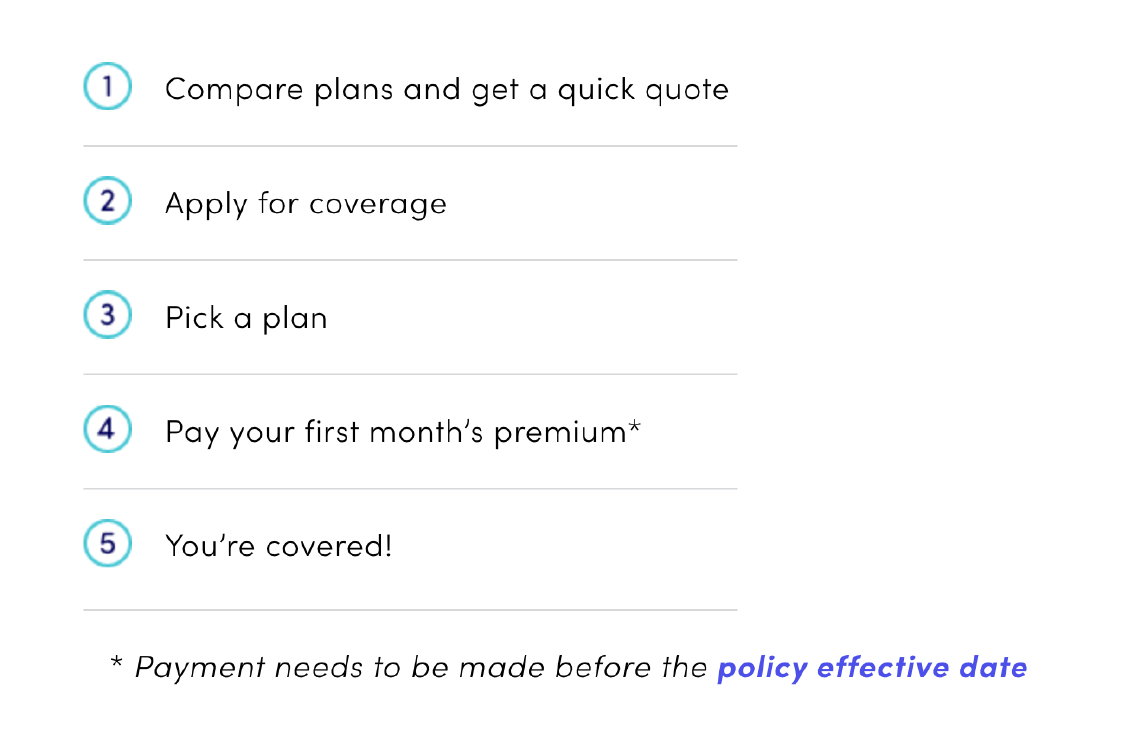
Follow these simple steps below to enroll in coverage through Pennie.
1. Preview – With our Plan Comparison Tool
-
- Get an estimate of your financial savings
- Compare health plans in your area
- Review each plan’s benefits and costs for health care services
2. Apply – Complete an application to find out your exact financial savings. Make sure you have your household information, tax forms, and other items in our Pennie Shopping Checklist.
3. Open Shopping Window – You will be asked to provide a Qualifying Life Event to shop for plans. Select “Loss of Medicaid/Medical Assistance (MA) or CHIP”.
4. Shop – Compare plans by costs and benefits and choose your plan (or confirm the plan you added to your “cart” in the preview step).
5. Pay – Your coverage cannot begin until you pay your first month’s premium before your policy effective date.
Note: If you apply for coverage through Pennie and you or someone in your household qualifies for Medical Assistance/Medicaid or CHIP, Pennie will transfer that individual’s account to the right program on their behalf. For enrollment assistance visit pennie.com/connect or call 1-844-844-8040. Pennie Customer Service is available Monday – Friday, 8:00 am – 6:00 pm.
Be sure to take action immediately if you have lost MA coverage. You have a limited time to enroll, and if you miss your enrollment window, you will need to wait until the next Pennie Open Enrollment period to get covered. Open Enrollment is every year from November 1 through January 15.
I currently have Medicaid coverage, what if I complete and return my renewal forms and am found ineligible?
If you are found ineligible for MA when your renewal is processed, you will get a notice in the mail telling you that your MA coverage is scheduled to end. You can appeal the decision if you believe it is not correct. Appeal and fair hearing rights and instructions for filing an appeal will be on the notice you will get.
If you are ineligible for MA, you may be referred to Pennie, Pennsylvania’s official health and dental insurance marketplace. You will receive a notice if you are referred to Pennie. Pennie lets you shop for plans available in your area and is the only place to get financial assistance to help pay for coverage and/or out-of-pocket costs.
Children under the age of 19 who are ineligible for MA may be referred to CHIP. CHIP provides high quality, affordable health coverage for families with children that covers all the care your child may need like doctors’ visits, prescriptions, vision, dental care, and more.
Visit the Department of Human Services Public Health Emergency webpage for more information: Public Health Emergency and Medical Assistance (pa.gov).
If I am found ineligible for Medicaid, will my information be automatically forwarded to Pennie and/or CHIP?
If you are found ineligible for Medicaid, your information may be automatically forwarded to Pennie and/or CHIP. However, if you do not receive any notice from either Pennie or CHIP, you can reach out through the contact information below.
Pennie
Online: www.pennie.com/connect
Phone: 1-844-844-8040
CHIP
Online: www.chipcoverspakids.com
CHIP Helpline: 1-800-986-KIDS (5437)
If I am found ineligible for Medicaid, what steps can I take to enroll through Pennie?
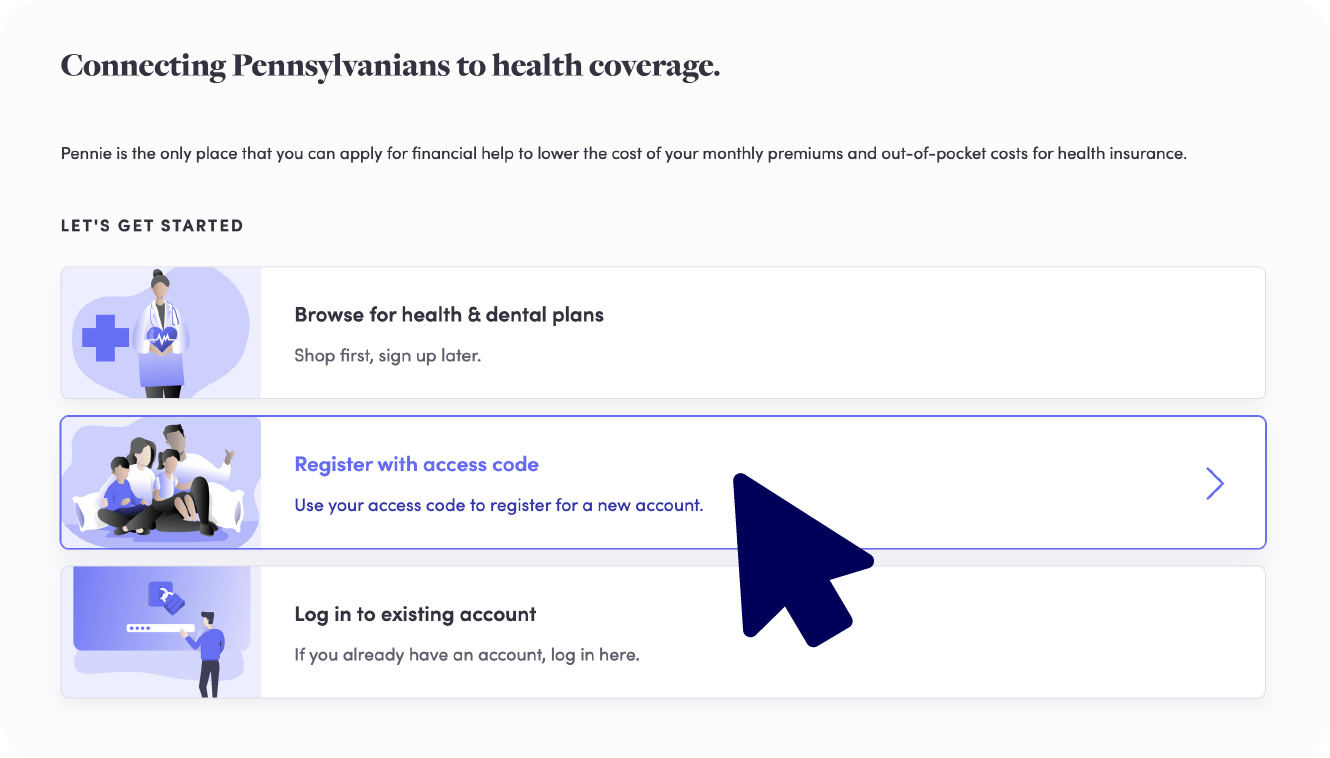
When you are found ineligible for Medicaid, your information will be automatically and securely transferred to Pennie or CHIP. Once transferred to Pennie, you will receive a notice with your account access information as well as details on the financial savings for which you qualify. Log in to your account by visiting enroll.pennie.com and using your new access code. After logging in, you may need to click through each page in your application to make sure your information is correct. If Pennie has enough information from MA, you may already see that the application is complete. You can then shop for the plan that best fits your needs. Your shopping window will be open, or you can select “Loss of Medicaid/Medical Assistance (MA) or CHIP” when asked.
If your application isn’t complete, you will receive a notice with information about how to complete your Pennie application.
IMPORTANT NOTE: Pick a health plan within 90 days from the date you lost Medicaid.
How can I find help enrolling in coverage through Pennie?
Option 1: Give us a call at the Pennie Customer Service Center at 1-844-844-8040 and work with our customer service team. Our team is trained to help you get the coverage that meets your needs. This multilingual team can answer tricky questions, direct you to online resources, and connect you to a Pennie-certified Broker or Assister to help you pick and pay for coverage.
Option 2: Contact a Pennie-certified Broker. Brokers are professionally trained to work with you one-on-one and can help narrow down options. Unlike other unbiased resources, Pennie-certified brokers can recommend the plan they feel is best suited for you and your family.
Option 3: Schedule an appointment with a Pennie-certified Assister. Our assisters are available to walk you through the shopping and enrollment process and have been trained to assist you both in-person or virtually.
Both brokers and assisters can be found on the Connect page at pennie.com.
For more information, visit pennie.com, check out our FAQs, or call 1-844-844-8040.
Find Answers. Meet Pros. Get Covered.
Pennie is here to help!
Pennie Certified Assisters, Brokers, and Customer Service Reps take you from Confused to Covered!

Call Us
We are ready to help and answer your questions!
Chat With Us
Looking for a quick answer? Check out our chat options.

Message Us
Have a general question? Send us a message.
Local Help
Find a Pennie-certified professional near you.